2025 New Medical Plan Vendor
UMR Login
To access the UMR website or app, see UMR Login for step-by-step instructions for logging in.
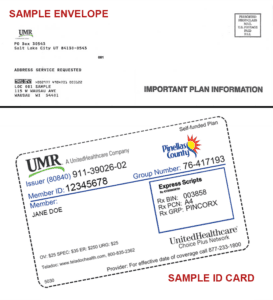
ID Cards
ID cards were mailed to your home in late December. No activation is required for your ID card. There are no rewards associated with activation.
GenYou by UMR
GenerationYou (GenYou) is an employee advocacy service offered by UMR that is tailored to you and your family’s unique medical care needs. When you call UMR, you will speak with a member of the GenYou team to help you with understanding your benefits, comparing providers, accessing cost estimates, scheduling appointments and much more.
As of January 1, 2025, Pinellas County changed vendors from Cigna to UMR, a UnitedHealthcare company, for employee medical and behavioral/mental health benefits and changed to Optum (a UMR/UnitedHealthcare company) for the Employee Assistance Program (EAP) plans.
There were no premium increases in 2025.
Spread the word by posting the printable flyer.
Click the question to read the answer to your top questions:
What changed?
As of January 1, 2025, the following benefits are provided by new vendors:
- Medical Plan: UMR (UnitedHealthcare)
- Behavioral/Mental Health Program: UMR (UnitedHealthcare)
- Employee Assistance Program (EAP): Optum (a UMR/UnitedHealthcare company)
Why was this change made?
UnitedHealthcare was our medical plan vendor prior to our transition to Cigna in 2022. As a result of ongoing employee feedback, we made the decision to move back to the UnitedHealthcare family, which was rated second place during the previous RFP process. This change is expected to cause minimal disruption and to provide larger provider networks.
What is the difference between UMR and UnitedHealthcare?
UMR (which stands for United Medical Resources) is a subsidiary of UnitedHealthcare. UMR serves as the administrator for self-funded medical plans such as the County’s. UMR will administer the plans and the network of health care providers will be the UnitedHealthcare Choice Plus network.
Am I paying more?
No. Your premium rates are the same in 2025 as 2024 for medical (includes prescription and vision) and dental.
Do I have a choice of two medical plans?
Yes. We offer a Preferred Provider Organization (PPO) Plan and a High Deductible Health Plan (HDHP) with a Health Savings Account.
Is my doctor in the new network?
We anticipate that almost all of your previous Cigna providers are in UMR’s UnitedHealthcare Choice Plus network. To verify if your doctor is in network:
- Visit www.UMR.com and select Find a Provider.
- Scroll down and in the search bar, type UnitedHealthcare Choice Plus for the network name and click Search.
- Scroll down and click the blue View Providers button for medical providers.
- Type the name of your doctor, medical group, or hospital in the search box.
- If you see In-Network Provider and a green checkmark below the name, they are included in the network.
- If your doctor is not listed, call their office and ask, “Do you accept UnitedHealthcare Choice Plus network?” If your doctor is not participating, you can encourage them to join the network.
- If you need help, contact Employee Benefits by email at employee.benefits@pinellas.gov or by phone at (727) 464-3367, option 1.
Note that the same network applies to both medical plans.
Is my behavioral/mental health provider in the new network?
To verify that your behavioral/mental health provider is in network:
- Visit www.UMR.com and select Find a Provider.
- Scroll down and in the search bar, type UnitedHealthcare Choice Plus for the network name and click Search.
- Scroll down and click the Behavioral Health Directory button for mental health and substance use providers such as therapists, psychiatrists, and clinics.
- Type the provider name in the search box and click Search.
- If the name is listed, they are included in the network.
- If your provider is not listed, call their office and ask, “Do you accept UnitedHealthcare Choice Plus network?” If they are not participating, you can encourage them to join the network.
- If you need help, contact Employee Benefits by email at employee.benefits@pinellas.gov or by phone at (727) 464-3367, option 1.
Note that the same network applies to both medical plans.
What if I don’t see UMR listed on my doctor’s website as an accepted insurance?
Look for UnitedHealthcare on your doctor’s website. UMR is unlikely to be listed as it is the third-party administrator for UnitedHealthcare.
When will I get an ID card?
ID cards were mailed to your home the week of December 23 which include your dependents’ names. You can request additional copies if needed. If you have more than 4 dependents, you will get two cards since there is a limit of 4 dependent names per card.
If you need your member and group ID numbers now, call UMR at (866) 783-6467 or call Employee Benefits at (727) 464-3367, option 1.
What if I’m under treatment for a health condition?
If you are under treatment for specific conditions such as cancer and it would be a hardship to change providers in the middle of treatment, there will be a 90-day transition period from January 1 to March 31, 2025 so that your care plan is not interrupted.
What if Cigna authorized a medical procedure or surgery for early 2025?
If your procedure or surgery was authorized prior to the end of the year, Cigna shared the information with UMR and it should be covered. If you have issues, please reach out to Employee Benefits by email at employee.benefits@pinellas.gov or by phone at (727) 464-3367, option 1.
Can I access the previous 2024 Cigna medical plans?
Yes. See the previous plans at Cigna Open Access Plus OAP Medical Plan Description and Cigna Open Access Plus HSA Medical Plan Description.
Are vision and prescription coverage included with medical plan coverage?
Yes. Your medical premium includes medical care, vision care, and prescription coverage. Although the medical plan vendor changed from Cigna to UMR (UnitedHealthcare), the prescription and vision vendors did not change.
Are there vendor changes for our other benefits?
No. The only benefits plans with a new administrator in 2025 are the medical plan, behavioral/mental health program, and Employee Assistance Program (EAP).
| Benefit | 2024 Vendor | 2025 Vendor |
|---|---|---|
| Medical | Cigna | UMR (UnitedHealthcare) |
| Behavioral/Mental Health | Cigna | UMR (UnitedHealthcare) |
| Employee Assistance Program (EAP) | Cigna | UMR (UnitedHealthcare) |
| Dental | Cigna | Cigna |
| Prescription | ExpressScripts | ExpressScripts |
| Vision | EyeMed | EyeMed |
| Life Insurance | Securian | Securian |
| Flexible Spending Accounts (FSA) | TASC | TASC |
| Short and Long Term Disability | UnitedHealthcare | UnitedHealthcare |
| FMLA | UnitedHealthcare | UnitedHealthcare |
| COBRA | iTedium | iTedium |
Are there onsite UMR representatives?
Yes. UMR is providing onsite representatives for claims assistance, health coaching, and Employee Assistance Program (EAP) services.
Are virtual visits available?
Yes. UMR (UnitedHealthcare) partners with Teladoc to offer 24/7 access to expert virtual care using a phone, tablet, or computer for your non-emergency medical and behavioral/mental health needs, including prescriptions.
Do we still have the Hinge Health Program?
Yes. We continue to offer the Hinge Health Program for employees enrolled in a Pinellas County medical plan. This free digital exercise therapy program supports muscle and joint health. Hinge Health provides a personalized therapy program and care team (via video and in-app messaging).
What about my rewards points for wellness?
Employees continue to accrue points for wellness activities, service anniversaries, and retirement. Our Rewards Program (login to SharePoint required) will not change. You will keep the points you’ve earned and may redeem them as desired. Starting in 2025, wellness rewards points will be tracked in a UMR (UnitedHealthcare) portal instead of MyCigna.
Is there still a Wellness Incentive Program?
Yes. We offer a Wellness Incentive Program through UMR (UnitedHealthcare), as we did with Cigna. The total rewards possible in 2025 are the same – $200 cash or 50,000 Rewards Program points.
Are there changes to retiree medical plans?
There is a vendor change for non-Medicare eligible retirees who are covered by UMR (UnitedHealthcare) instead of Cigna as of January 1, 2025. Our Medicare-eligible retirees continue to be covered by Aetna’s Medicare Advantage plan.
What if I have more questions?
Call UMR at (866) 783-6467 or contact Employee Benefits by email at employee.benefits@pinellas.gov or by phone at (727) 464-3367, option 1.
2/19/25